Gardnerella Vaginalis: Causes, Symptoms, Risks & Treatment
Last updated: Nov 18, 2025
| Test Options |
|
| Treatment | Oral or intravaginal antibiotics |
| Price |
|
| Appointment Options |
Same-day appointment (subject to availability). Book via WhatsApp: 8877 0326 or email: hi@atamed.sg |
| Clinic Locations |
Orchard: 1 Orchard Blvd
#05-09 Camden Medical Centre, S248649 Tanjong Pagar: 72 Anson Rd #01-02 Anson House, S079911 |
What Is Gardnerella Vaginalis?
Gardnerella vaginalis (G. vaginalis) is a type of bacteria that lives in the
vagina and is most commonly linked to bacterial vaginosis (BV), a condition
caused by the overgrowth of G. vaginalis along with other bacteria when the natural balance
of the vaginal microbiome is disrupted.
Normally, the vagina contains mostly helpful bacteria, especially lactobacilli, which keep it
healthy and slightly acidic. When Gardnerella grows too much, it can reduce the number of
these helpful bacteria and cause symptoms such as unusual discharge and a strong smell.
If left untreated, it may increase the risk of infections, complications during
pregnancy, and other reproductive health issues.
Gardnerella Vaginalis Causes
An overgrowth of G. vaginalis usually occurs when the number of protective
lactobacilli in the vagina decreases due to biological, behavioural, or environmental
factors. This disruption allows G. vaginalis and other bacteria to multiply more
easily.
Common contributing factors include:
- Frequent vaginal douching.
- Unprotected sex with multiple partners.
- Use of antibiotics that disturb the vaginal microbiome.
- Hormonal changes, especially during menstruation or pregnancy.
These factors can lower vaginal acidity, weakening the body's natural defences that normally keep
G. vaginalis under control.
Although G. vaginalis is not classified as a traditional sexually
transmitted infection (STI), sexual activity plays an important role in its transmission and
recurrence. It is more common in sexually active individuals and may be influenced by new or
multiple sexual partners. However, it can also occur in people with no recent sexual activity.
Gardnerella Vaginalis Symptoms
An overgrowth of G. vaginalis commonly results in BV, which may cause a range of noticeable symptoms. The most frequent signs include:
- Thin, grey or white vaginal discharge
- A strong, fish-like odour, especially after sexual intercourse
- Vaginal itching or irritation
- A burning sensation during urination
However, some individuals may have no symptoms, particularly in the early stages or when bacterial levels are low.

What Are the Risks of Untreated Gardnerella Vaginalis?
If left untreated, an overgrowth of G. vaginalis can increase the risk of several health complications. These may include:
- Greater susceptibility to sexually transmitted infections (STIs) – The imbalance weakens the vagina’s natural defences, making it easier for harmful bacteria and viruses to enter.
- Pregnancy-related issues – Inflammation may affect the uterus and surrounding tissues, increasing the risk of preterm birth and low birth weight.
- Post-surgical infections, particularly following gynaecological procedures – A disrupted balance of vaginal bacteria can raise the risk of infection after procedures such as IUD insertion or abortion.
- Pelvic inflammatory disease (PID) – Bacteria can spread from the vagina into the uterus and fallopian tubes, leading to inflammation and potential long-term complications.
How Is Gardnerella Vaginalis Diagnosed?
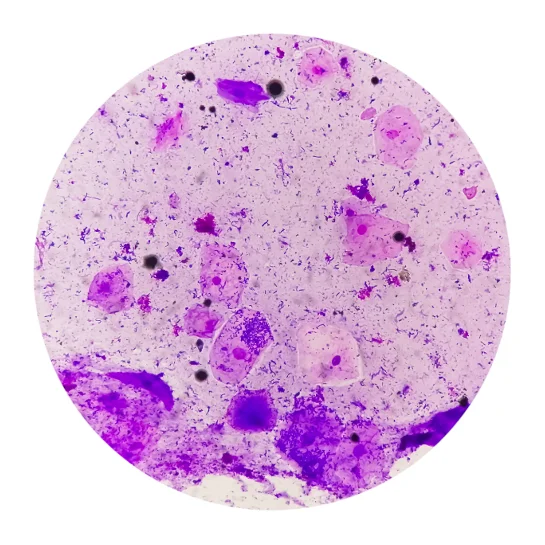
G. vaginalis is diagnosed through a combination of symptom assessment and swab-based clinical tests designed to confirm BV. A vaginal swab is typically used to perform several of the following methods:
- Microscopy – The swab sample is examined under a microscope to look for "clue cells," which are vaginal cells coated with bacteria.
- pH Testing – The swab is used to measure vaginal pH, and a result above 4.5 suggests an imbalance in the vaginal environment.
- Whiff Test – A drop of potassium hydroxide is added to the swab sample; the release of a strong, fishy odour may indicate bacterial overgrowth.
- Nucleic Acid Amplification Tests (NAATs) – This lab-based test detects G. vaginalis DNA with high sensitivity and is often used when more precise identification is required.
Gardnerella Vaginalis Treatment
An overgrowth of G. vaginalis is typically treated with antibiotics that target the
bacterial imbalance causing BV.
Commonly prescribed antibiotics (oral or intravaginal) include:
In some cases, particularly with recurrent BV, additional strategies may be recommended. These may include the use of probiotics to support the growth of healthy vaginal bacteria or follow-up consultations to explore contributing factors such as sexual activity or hygiene practices.
Gardnerella Vaginalis Testing & Treatment Cost
At ATA Medical, we offer diagnostic testing for bacterial vaginosis caused by G. vaginalis, along with appropriate treatment when required. Our prices are as follows:
| Test / Treatment | Test Type | Price* |
|---|---|---|
| Consultation | From $49.05 | |
|
DNA Probe/Multiplex Real Time PCR for Vaginitis Gardnerella vaginalis, Candida albicans and Trichomonas vaginalis** |
Swab | $147.15 |
|
Basic Female Genital Screen (5 tests) Chlamydia PCR, Gonorrhoea PCR, Candida, Gardnerella Vaginosis, Trichomonas |
Swab | $268 |
|
Enhanced Female Genital Screen (9 tests) Chlamydia, Gonorrhoea, Mycoplasma genitalium, Mycoplasma hominis, Trichomonas, Ureaplasma parvum, Ureaplasma urealyticum, Candida, Gardnerella Vaginosis |
Swab | $348 |
|
Complete Female STD Screen (15 tests) HIV, Syphilis, Hepatitis B, Hepatitis C, Herpes Simplex Virus 1 and 2, Chlamydia, Gonorrhoea, Mycoplasma genitalium, Mycoplasma hominis, Trichomonas, Ureaplasma parvum, Ureaplasma urealyticum, Candida, Gardnerella Vaginosis |
Blood + Swab | $478 |
| Oral Antibiotics | From $0.87 per tab | |
| Intravaginal Antibiotics | $59.95 per box | |
^Prices last updated on Jan 28, 2026. While every effort is made to keep pricing information up to date, please contact our team to confirm the latest rates.
**These tests have higher sensitivity and are recommended for more accurate results.
We also provide a full range of STI
testing and women’s
health services. Female doctors are available on request to support your comfort throughout
the consultation and testing process.
Contact us to learn more or to book an
appointment.
Gardnerella Vaginalis Prevention
Preventing an overgrowth of G. vaginalis involves supporting the natural balance of bacteria in the vagina and avoiding behaviours that may disrupt it. Key prevention strategies include:
- Avoiding vaginal douching, which can interfere with the vagina’s natural bacterial balance.
- Completing prescribed antibiotic courses fully to help prevent bacterial overgrowth.
- Using condoms during sexual activity to reduce the spread of potentially disruptive bacteria.
- Limiting the number of sexual partners, as frequent changes may influence vaginal health.
- Wearing breathable, cotton undergarments to help keep the area dry and minimise irritation.
How Do I Book a Gardnerella Vaginalis Testing Appointment?
ATA Medical @ Orchard
Nearest MRT: Orchard Boulevard Station (TE13)
Contact Number: 6223 0682
Email: camden@atamed.sg
Opening Hours:
Mon - Fri: 8:30 AM to 12:30 PM, 1:30 PM to 5:30 PM
Sat: 8:30 AM to 12:30 PM
Sun & PH: Closed
ATA Medical @ Tanjong Pagar
Nearest MRT: Tanjong Pagar Station (EW15)
Contact Number: 6223 0682
Email: hi@atamed.sg
Opening Hours:
Mon - Fri: 8:30 AM to 12:30 PM, 1:30 PM to 5:30 PM
Sat: 8:30 AM to 12:30 PM
Sun & PH: Closed


