What Is a Vaginal Yeast Infection?
A vaginal yeast infection, also known as vaginal
candidiasis or thrush, is a common fungal infection caused
by the overgrowth of Candida species, particularly Candida
albicans. While small amounts of Candida naturally exist in the
vagina, certain conditions can disrupt the microbial balance, leading to an
infection.
This condition typically results in symptoms such as itching, burning,
abnormal vaginal discharge, and irritation around the vaginal area. These
symptoms can interfere with daily activities, including work, sleep, and
sexual comfort.
Vaginal yeast infections are not considered sexually transmitted infections
(STIs), although they can occasionally be triggered by sexual
activity or transmitted between partners.

What Are the Common Symptoms?
Symptoms of a vaginal yeast infection usually involve irritation, unusual discharge,
and discomfort, though the severity can vary from person to person.
Typical symptoms include:
- Itching and irritation around the vaginal and vulval areas
- Thick, white vaginal discharge that resembles cottage cheese
- Redness and swelling of the vulva
- General soreness or discomfort in the vaginal area
- Burning sensation during urination or sexual intercourse
Some individuals may experience only mild symptoms, while others may find that the condition significantly affects their daily comfort and activities.
Vaginal Yeast Infections Causes
Vaginal yeast infections can arise from various biological, behavioural, and
environmental factors that disrupt the natural balance of microorganisms in
the vagina.
Common causes include:
- Antibiotic use – Certain antibiotics can reduce the healthy bacteria in the vagina that normally help keep Candida under control.
- Hormonal fluctuations – Changes during pregnancy, use of oral contraceptives, or hormone replacement therapy can affect the natural balance of bacteria and yeast in the vagina.
- Use of harsh hygiene products – Scented soaps, douches, and vaginal sprays can disturb the vaginal environment.
- Tight or non-breathable clothing – Prolonged moisture and warmth can create favourable conditions for fungal growth.
- Poorly controlled diabetes – Elevated blood sugar levels may encourage fungal overgrowth.
- Weakened immune system – Individuals with conditions such as HIV or those undergoing immunosuppressive therapy may be more susceptible.
- Sexual activity or reinfection from a partner – While vaginal yeast infections are not considered STIs, sexual activity may sometimes trigger symptoms or contribute to recurrence in some individuals.
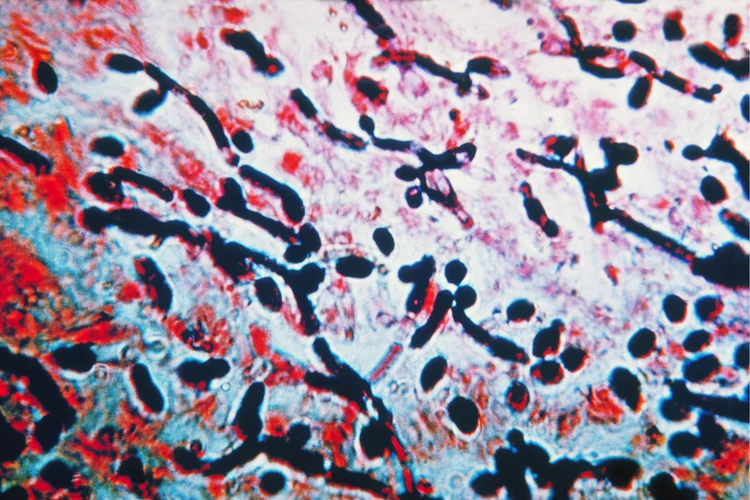
How Is a Vaginal Yeast Infection Diagnosed?
Diagnosing a vaginal yeast infection typically involves a clinical evaluation and,
when necessary, laboratory testing to confirm the presence of Candida.
This may include:
- Reviewing your medical history and symptoms, including any previous infections, recent antibiotic use, hormonal changes, or underlying health conditions such as diabetes.
- Performing a pelvic examination, to check for signs of inflammation, discharge, or irritation.
- Taking a vaginal swab, for microscopic examination or culture.
Because symptoms can resemble those of other conditions such as bacterial vaginosis, trichomoniasis, or STIs, precise diagnosis is important to guide appropriate treatment.
How to Treat a Vaginal Yeast Infection?
Treatment for vaginal yeast infections typically involves antifungal medications,
which may be applied locally to the vaginal area or taken orally, depending on the
severity and frequency of the infection.
Common treatment approaches include:
- Topical antifungal creams or suppositories (e.g., clotrimazole or miconazole) – Applied over the vulva or inserted into the vagina for several days to reduce fungal overgrowth.
- Oral antifungal medication (e.g., fluconazole) – Usually prescribed as a single-dose for uncomplicated cases.
- Combination therapies – May be recommended for more severe or recurrent infections (typically defined as four or more episodes within a 12-month period), involving both topical and oral treatments over an extended course.
- Addressing underlying factors – Managing issues such as poorly controlled diabetes, hormonal imbalances, or potential reinfection from a sexual partner can support long-term resolution and help prevent recurrence.

Your doctor will recommend the most appropriate treatment based on your medical history, frequency of infections, and specific symptoms.
Vaginal Yeast Infection Diagnosis & Treatment Cost
At ATA Medical, we offer diagnosis and treatment for vaginal yeast infections, along with other women’s health services.
| Test / Treatment | Test Type | Price* |
|---|---|---|
| Consultation | From $49.05 | |
| Testing | ||
|
DNA Probe/Multiplex Real Time PCR for Vaginitis Gardnerella vaginalis, Candida albicans and Trichomonas vaginalis |
Swab | $147.15 |
|
Basic Female Genital Screen (5 tests) Chlamydia PCR, Gonorrhoea PCR, Candida, Gardnerella Vaginosis, Trichomonas |
Swab | $268 |
|
Enhanced Female Genital Screen (9 tests) Chlamydia, Gonorrhoea, Mycoplasma genitalium, Mycoplasma hominis, Trichomonas, Ureaplasma parvum, Ureaplasma urealyticum, Candida, Gardnerella Vaginosis |
Swab | $348 |
|
Complete Female STD Screen (15 tests) HIV, Syphilis, Hepatitis B, Hepatitis C, Herpes Simplex Virus 1 and 2, Chlamydia, Gonorrhoea, Mycoplasma genitalium, Mycoplasma hominis, Trichomonas, Ureaplasma parvum, Ureaplasma urealyticum, Candida, Gardnerella Vaginosisurealyticum, Candida, Gardnerella Vaginosis |
Blood + Swab | $478 |
| Treatment | ||
| Topical Antifungal Cream | From $10.90 | |
| Pessary Antifungal Cream | $59.95 for full course of treatment | |
| Oral Antifungal Medication | From $1.41 per tab | |
^Prices last updated on Jan 28, 2026. While every effort is made to keep pricing information up to date, please contact our team to confirm the latest rates.
We offer confidential testing and treatment
for STIs, available either as individual tests or part of comprehensive
screening packages. To support your comfort and preferences, both male and female
doctors are available upon request.
For details on available tests, treatment options, or to schedule an appointment,
please contact us directly.
How Can You Prevent Vaginal Yeast Infections?
You can lower your risk of developing vaginal yeast infections by adopting habits
that support vaginal health and help maintain a balanced microbial environment.
Preventive measures can include:
- Maintaining good personal hygiene without excessive washing or the use of harsh products.
- Avoiding scented hygiene products and douches, which can disrupt the natural balance in the vagina.
- Wearing breathable, cotton, and looser-fitting clothing to reduce heat and moisture retention.
- Changing out of damp exercise clothing or swimwear promptly to minimise moisture build-up.
- Using antibiotics only when necessary and completing the prescribed course.
- Managing blood sugar levels if you have diabetes.
When Should You See a Doctor?
You should consult a doctor if:
- You suspect a vaginal infection or are experiencing symptoms such as foul-smelling discharge, fever, abdominal pain, bleeding unrelated to your period, or pain during intercourse.
- You have recurrent infections.
- You experience persistent itching or notice unusual changes in vaginal discharge despite treatment.
A proper diagnosis is important for guiding appropriate treatment, especially since other conditions such as bacterial vaginosis, STIs, or dermatological issues can present with similar symptoms.
Why Choose ATA Medical?








Making a Difference Together
At ATA Medical, we strive to make a meaningful impact on every patient's health. With over 150,000 patients served, we are dedicated to fostering trust and enhancing well-being across our community.
Patients
Health Screening Tests
Corporate Screenings
Delivering Care Patients Appreciate
What to Expect
FAST RESULTS
We strive to deliver your results within 7 working days.
MINIMUM WAITING TIME
Our patient-oriented processes ensure your waiting time is kept to a minimum.
Friendly Service
Service is a top priority for us at ATA Medical.
Email Us at camden@atamed.sg
for More Information.
Book Your Vaginal Yeast Infection Treatment With Us at 88750352.

